Looking for a trauma therapist in Denver?
Over half of all Americans will experience a traumatic event during their lifetime. If the trauma happened in childhood--things like abuse, neglect, or sudden loss of a loved one—it can have life-long effects. But many of these effects of trauma can be decreased or reversed with treatment.
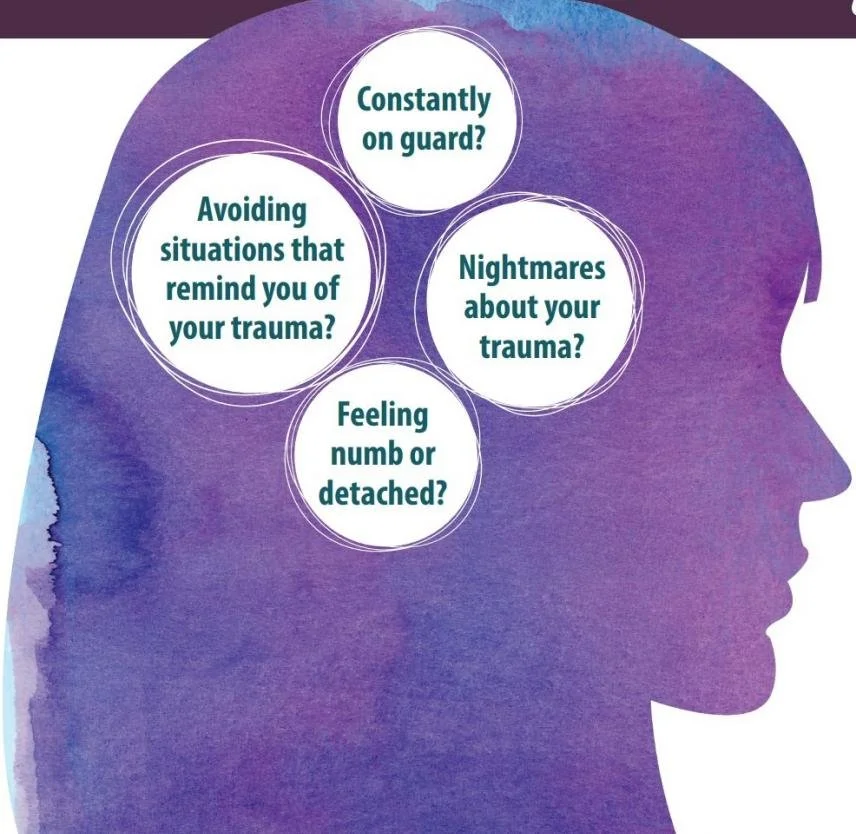
When people ask if they have post traumatic stress disorder, or PTSD, the first thing I tell them is that any person who experiences a traumatic event may get a range of normal, predictable reactions. Things like uncontrollable thoughts about the event, replaying it over-and-over, self-doubt, self-judgment, jumpiness, nightmares, physical ailments, and even feelings of fear and isolation are all very unpleasant, normal reactions to trauma.
For many people these symptoms decrease and pass within a few weeks. But for 20% of people (and that’s a lot of people!) the symptoms persist, they get worse, or they show up later, bringing a sense of confusion like, “I thought I was over this!” This is called PTSD, when a person gets stuck in the healing process and with these very uncomfortable symptoms.
This .pdf from the National Institute of Mental Health gives a comprehensive list of the symptoms of PTSD. These symptoms can get so unbearable that a person may start drinking or using substances to cope. They may cut off from family and friends. Or the opposite—people may go out even more, have quick, risky relationships, or throw themselves into work so that they don’t have to think about the terrible thing that happened. These trauma symptoms—and our exhausting efforts to manage them—squeeze and shrink our lives, cause depression and anxiety, make us question our self-worth, or even question the point of living. But we can fight back. With help from a trauma-focused therapist, PTSD is diagnosable, treatable, and beatable.
Treatment for PTSD
There are several evidence-based treatments for PTSD, methods that have been studied in blind clinical trials with repeatable results that show their effectiveness in getting positive outcomes for trauma survivors. These methods include: Cognitive Behavioral Therapy (CBT), Trauma Focused Cognitive Behavioral Therapy (TF-CBT), Cognitive Processing Therapy (CPT), Eye Movement and Desensitization and Repossessing (EMDR), and Prolonged Exposure. There are more, but these are the models the most recommended by the American Psychiatric Association.
As a trauma therapist in Denver, I use the models CPT (for adults) and TF-CBT (for kids, teens, and young adults). I have formal training in both methods, and I have seen successful outcomes in patients firsthand. I write about these different methods, how they work, and what’s involved for participants in my blog post (link here).
What if my child has gone through trauma?
The National Child Traumatic Stress Network (NCTSN) was formed after the events of 9/11/2001 to study and address the specific needs of children who’ve been effected by trauma. I received graduate level training from NCTSN at the Silberman School of Social Work in New York City, where I studied about the special needs of kids who are trauma survivors.
Kids and teens experience traumas in different ways than adults, and they require different treatment. The human brain is not completely developed until around 25-years old. And at each stage of development our brains are working hard on mastering different tasks and skills. Trauma can (not always but often) interrupt the development process and prevent the child from reaching full potential until the trauma is addressed. This interruption often effects behavior at home and at school, peer and family relationships, and academic performance. All these troubles have cascading effects on the child’s environment, they change the reactions from caregivers, teachers, friends, the way the child sees themselves. We call these cascading effects because one leads to another and then to another, and then to another.
Let’s look at an example:
Dustin (a fictional case study). Dustin is a 9-year old boy who loves going to school and seeing friends. When he gets home he likes to play computer games and card games in his room. He gets along with siblings well most of the time and doesn’t even mind doing a chore here and there when asked. On his way to school one day, the bus got in a bad accident and turned on its side. Nobody was seriously hurt, and the incident was was put behind them. About a month later, Dustin’s parents notice shifts in his behavior. He starts fighting with siblings more, gets in detention at school, falls back on grades, and in an outburst one evening he breaks his video game controller. Nobody knows what to do, so discipline is tried first. Video games are restricted, and study time is enforced. Soon Dustin is failing a class. He’s isolating in his room. A visit to the doctor gets him ADHD medication, and he’s feeling like all the conflict in the house is his fault. One day when his teacher doesn’t let him go to the bathroom during a test, Dustin wets his pants. Due to this accident, he is bullied on the playground. Dustin is afraid to go to school now and cries in the mornings, complains of stomach problems, and begs his parents to let him stay home.
This story illustrates how, left untreated, the symptoms of trauma can cause other unforeseen consequences which then create their own set of problems on top of the trauma symptoms. With each layer the original cause is less and less obvious. When working with children who have experienced trauma, the first step is to get all the stakeholders on the same page. A therapist can connect with parents, babysitters, teachers, school counselors, and coaches, to educate them and help provide a nurturing, supportive net to hold and protect the child as they do their healing work in therapy, at home, and in the community. You can learn more about the method I use for treating teens and kids at my blog post at this link.
Asking for help to face trauma can be extremely difficult for families. Sometimes there’s a sense of shame around what happened, as in the case of sexual abuse. We may feel drawn to say “let’s wait and see if they get over it on their own.” But we know that trauma thrives in the dark. Keeping it silent or secret makes it grow. It can eventually take over every part of a persons life, leading to more difficulties and troubles for the family to contend with on their journey.
Getting help is hard!
Imagine it like this. A kiddo falls off their bike and they get a big scrape on their knee. It’s tempting to slap on a band aid and move on. But what could happen if we leave it alone? It might get infected. It could get so infected that we have to go to the hospital, take medicine, or possibly lose the leg altogether! That’s how trauma becomes the infection of our lives. If we cover it up and “just move on” without tending to the wound, it can fester and cause way more trouble down the line. Instead, what do we do when we get a big scrape? We first have to look at it. We have to go in, gently, and clean the wound, take out the gravel and dirt. We have to disinfect it, maybe put on some cream to sooth it and help it heal. And then we have to change the bandage regularly to keep it clean. This is trauma focused treatment. It’s intentional, careful work to heal the wound before it becomes something too big to handle.
Kids show incredible courage when we let them. They tend to believe in themselves when we show them that we believe in them. When we have the courage to stand beside them and witness their pain, then they can persevere, heal, and flourish, confident in their own strength and the knowledge that they are not alone.
...

“The lotus flower blooms most beautifully from the deepest and thickest mud.”
– Buddha
Articles and Resources
-

Veteran's Association
The Veteran’s Administration’s page on PTSD and the recommended treatments
-

American Psychiatric Association
The APA’s official recommended treatments for PTSD.
-

Support through Groups
Follow this link for support and resources that take your insurance through the search function of Psychology Today.